Book Your Consultation With Nulife IVF Clinic
Share your details and our team will help you schedule an appointment with Navi Mumbai's best IVF Clinic
- Home
- / Our Specialities
- / Sperm Retrieval (TESA, TESE, PESA, MESA)
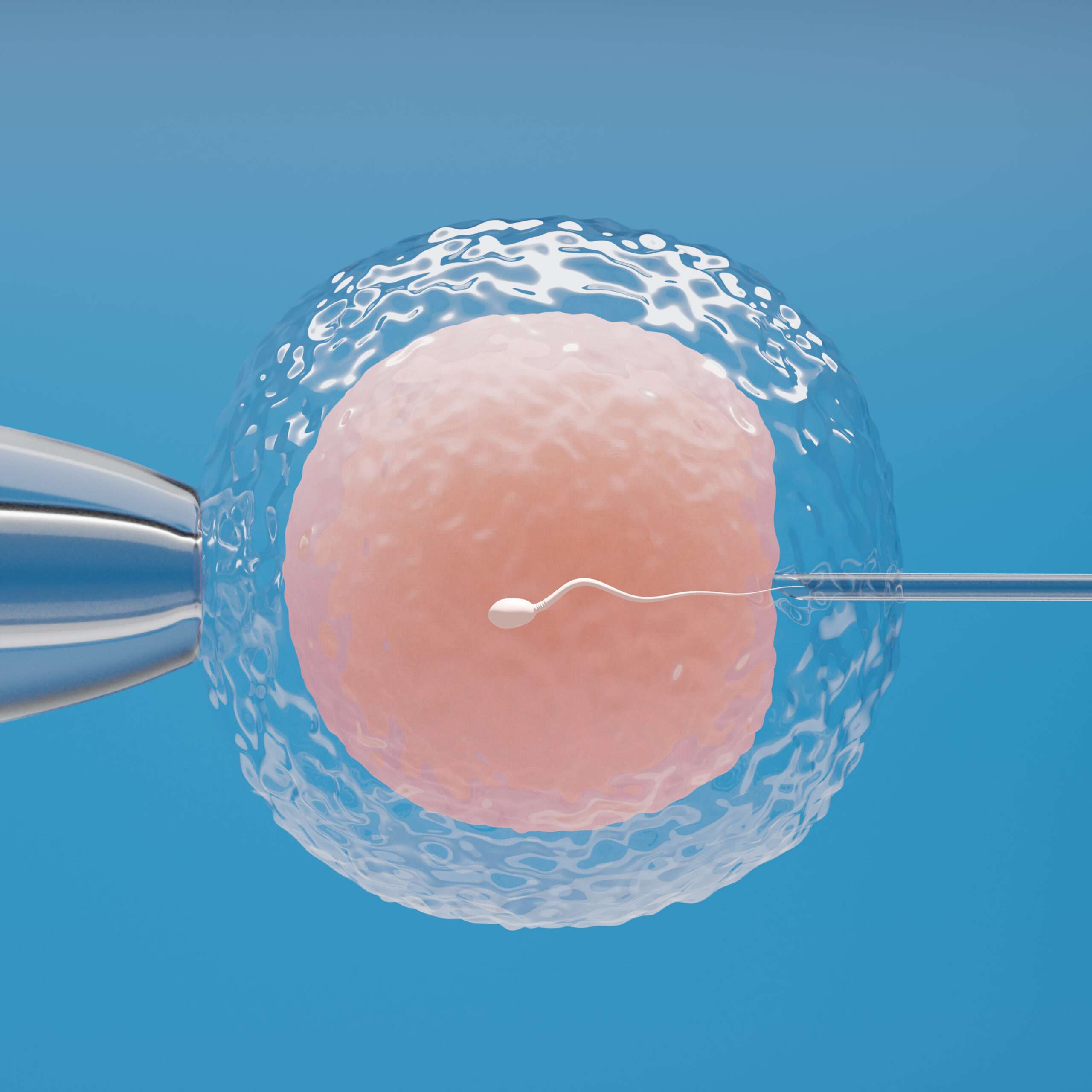
Sperm Retrieval (TESA, TESE, PESA, MESA) at Nulife IVF
Advanced surgical sperm retrieval techniques at Nulife IVF Clinic helping men with azoospermia or severe sperm problems.
What Is Sperm Retrieval?
Sperm retrieval refers to a set of minimally invasive procedures designed to collect viable sperm directly from the testicles or epididymis when sperm is absent in the ejaculate. This condition, known as azoospermia, can be caused by a blockage in the reproductive tract, prior vasectomy, or severely reduced sperm production. Sperm retrieval allows men who would otherwise be unable to father children naturally to achieve biological parenthood.
At Nulife IVF Clinic in Seawoods, Navi Mumbai, we use modern microsurgical techniques such as TESA (Testicular Sperm Aspiration), TESE (Testicular Sperm Extraction), PESA (Percutaneous Epididymal Sperm Aspiration), and MESA (Microsurgical Epididymal Sperm Aspiration). These procedures are performed by highly experienced male fertility specialists and embryologists, ensuring maximum sperm recovery with minimal discomfort.
Why Choose Nulife IVF Clinic for Sperm Retrieval in Navi Mumbai
- Comprehensive Male Fertility Care: Every patient receives a thorough evaluation, including hormone testing, semen analysis, scrotal imaging, and detailed consultation. Based on these findings, we recommend the most suitable retrieval method tailored to the individual’s needs.
- Advanced Microsurgical Expertise: Our team of urologists and embryologists uses precision microsurgical techniques to handle testicular or epididymal tissue gently. This ensures the highest chance of retrieving viable sperm while preserving testicular function.
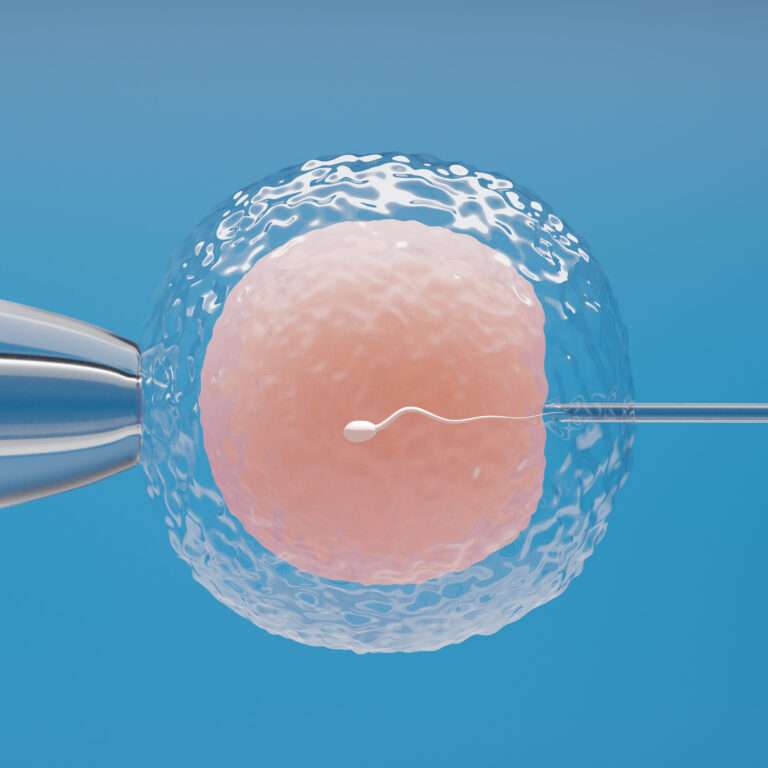
- Integration with IVF & ICSI: Retrieved sperm can be used immediately for ICSI or IVF in our state-of-the-art laboratory, improving fertilization success. In some cases, excess sperm is cryopreserved for future cycles, offering flexibility.
- Patient-Centered Approach: At every stage, from consultation to recovery, we prioritize comfort, privacy, and emotional support. Our team guides patients and their partners, addressing concerns and providing reassurance throughout the process.
Types of Sperm Retrieval Procedures
-
TESA – Testicular Sperm Aspiration
TESA involves inserting a fine needle into the testicle to aspirate small tissue samples. These samples are examined in the lab for viable sperm. The procedure is quick, minimally invasive, and usually performed under local anesthesia. -
TESE – Testicular Sperm Extraction
TESE is a minor surgical biopsy of testicular tissue. It is especially useful in cases of non-obstructive azoospermia, where sperm production is low but present in small pockets within the testicle. Multiple samples may be taken to maximize retrieval chances. -
PESA – Percutaneous Epididymal Sperm Aspiration
PESA is performed by inserting a needle into the epididymis to extract sperm. It is ideal for men with obstructive azoospermia caused by a vasectomy or blockages in the reproductive tract. -
MESA – Microsurgical Epididymal Sperm Aspiration
MESA is a more precise technique, performed under an operating microscope. It allows the embryologist to collect sperm directly from the epididymis with minimal tissue trauma. This method is preferred for men who have undergone vasectomy or have congenital blockages.
All these procedures are typically performed as day-care surgeries. Patients can usually return home the same day, and recovery is generally quick with minimal discomfort.
When Is Sperm Retrieval Recommended?
Sperm retrieval is advised in the following situations:
- Obstructive azoospermia: Caused by vasectomy, congenital absence of the vas deferens, or blockage in the ejaculatory ducts.
- Non-obstructive azoospermia: Very low or absent sperm production due to testicular dysfunction.
- Failed vasectomy reversal or persistent blockages: When prior corrective surgery does not restore sperm in the ejaculate.
- Severe testicular injury or infection: Cases where sperm cannot naturally reach the ejaculate.
- Fertility preservation: Men undergoing cancer treatment or other medical therapies that may affect sperm production.
Success Rates and Benefits
The success of sperm retrieval depends on the underlying condition and the technique used. At Nulife IVF Clinic, many men with azoospermia have successfully fathered children through retrieved sperm combined with ICSI.
Key benefits include:
- Enables biological fatherhood even when no sperm is present in the semen.
- Minimally invasive procedures with short recovery times.
- Can be combined immediately with IVF or ICSI for maximum fertilization chances.
- Cryopreservation of retrieved sperm offers flexibility for future use.
- Safe and effective when performed by skilled specialists in a modern clinical environment.
Our Process at Nulife IVF Clinic
-
Initial Assessment
The journey begins with a detailed evaluation, including semen analysis, hormone tests, scrotal ultrasound, and a complete medical history review. This ensures the right retrieval method is selected. -
Procedure Planning
Based on findings, we recommend the most suitable technique: TESA, TESE, PESA, or MESA. Patients are informed of the benefits, risks, and recovery expectations before proceeding. -
Sperm Retrieval
The selected procedure is performed under local or short general anesthesia. Tissue or fluid is carefully handled and sent to the embryology lab to isolate viable sperm. -
Sperm Processing & Storage
Retrieved sperm is either used immediately for ICSI or IVF or cryopreserved for future use. Our laboratory ensures optimal handling to maintain sperm viability and maximize the chance of fertilization. -
Follow-Up and Fertility Support
Patients are monitored post-procedure for recovery and advised on timing for assisted reproductive cycles. Counseling and guidance are provided to support emotional well-being throughout the fertility journey.
Sperm retrieval offers hope to men with no sperm in their ejaculate, allowing them to achieve biological parenthood. At Nulife IVF Clinic, our expertise, advanced lab facilities, and patient-centered approach ensure a safe, effective, and supportive experience. By combining microsurgical techniques with state-of-the-art ART procedures, we maximize the chances of conception while prioritizing comfort, privacy, and overall reproductive health.
Our Specialities
- Male infertility workup
- Female Infertility Work-up and Treatment
- IUI (intrauterine insemination)
- IVF (In Vitro Fertilization)
- ICSI (Intracytoplasmic Sperm Injection)
- Sperm Retrieval (TESA, TESE, PESA, MESA)
- Varicocelectomy
- Tuboplasty for Tubal Block
- Timed Intercourse
- Follicular / Ovulation Study
- Frozen Embryo Transfer (FET)
- Oocyte Retrieval
- View All Specialities
Hospital Locations
Nulife IVF, Seawoods, Navi Mumbai
Success Stories from Our Patients
Couples share their journey to parenthood with Nulife IVF Clinic.
I consulted Dr. Priyal for a IVF issue I had been anxious about for months, and I’m so glad I did. She made a sensitive topic easy to talk about...

Frequently Asked Questions About Sperm Retrieval
TESA and TESE involve collecting sperm directly from the testicles. TESA uses a needle to aspirate small tissue samples, while TESE performs a minor biopsy to extract tissue. PESA and MESA collect sperm from the epididymis; MESA is performed under a surgical microscope, allowing precise retrieval with minimal tissue damage. The choice depends on sperm production, obstruction type, and prior procedures.
The procedures are performed under local or short general anesthesia, ensuring minimal discomfort during the process. Afterward, mild soreness, swelling, or bruising may occur, which typically resolves in 1–2 days. Pain management and post-procedure guidance are provided to ensure a comfortable recovery.
Sperm retrieval is recommended for men with azoospermia (no sperm in ejaculate), obstructed ducts due to vasectomy or congenital conditions, severely low sperm count, or those who have undergone unsuccessful fertility treatments. It is also advised when sperm is required for IVF/ICSI but cannot be obtained naturally.
No. Retrieved sperm often have limited motility and are collected directly from the testicle or epididymis. These sperm are not suitable for natural conception and are instead used with ICSI or IVF procedures to fertilize eggs in a laboratory setting.
If eggs are available on the same day, fertilization via ICSI can proceed immediately. Otherwise, sperm can be cryopreserved and used in future IVF/ICSI cycles, providing flexibility and avoiding the need for repeated surgical procedures.
Sperm retrieval is generally safe. Minor complications include local swelling, bruising, or temporary discomfort. Rarely, infection, bleeding, or hematoma may occur, but these are usually manageable with standard medical care. Your specialist monitors recovery to minimize risks.
Success depends on the underlying cause of azoospermia and testicular health. Obstructive azoospermia has higher retrieval success compared to non-obstructive cases. Your fertility specialist will assess testicular function, prior procedures, and overall health to provide realistic expectations for sperm retrieval outcomes.
Yes. Cryopreservation allows retrieved sperm to be stored for future use, enabling multiple IVF/ICSI cycles without repeating surgery. This is particularly useful when coordinating with egg retrieval or preserving fertility before medical treatments that may affect sperm production.
No. Only small amounts of tissue are removed during TESA, TESE, PESA, or MESA. In most cases, testicular function and testosterone levels remain normal. Regular monitoring ensures hormone levels stay within healthy ranges post-procedure.
Yes. If some sperm-producing cells remain in the testes, techniques like TESA or TESE can retrieve viable sperm, even after chemotherapy or radiotherapy. Cryopreservation may also be offered before treatment as a preventive measure for fertility preservation.
Recovery is generally quick. Most men resume light activities or office work within 24–48 hours. Strenuous exercise or heavy lifting should be avoided for 1–2 weeks. Pain or discomfort typically subsides within a few days, and follow-up consultations ensure proper healing.
Yes. If retrieval is unsuccessful, options such as donor sperm for ICSI or IVF, adoption, or fertility counseling can be considered. Our specialists provide personalized guidance and emotional support to explore the best possible path to parenthood.
Book Your Consultation for Male Fertility Treatment at Nulife IVF Clinic
At Nulife IVF Clinic, Seawoods, Navi Mumbai, our team combines advanced surgical skills, embryology expertise, and supportive counseling to help men with complex fertility challenges. Using TESA, TESE, PESA, or MESA, we aim to provide the best chance at achieving fatherhood.
Your Guide to Advanced Male Fertility Care at Nulife IVF Clinic
Explore sperm retrieval, ICSI, and other ART options designed to help men achieve successful parenthood.

ICSI (Intracytoplasmic Sperm Injection)
IVF (In Vitro Fertilization)

Fertility-Enhancing Endoscopic Surgeries
Get in Touch with Our Fertility Experts!
Contact Us for Appointments and Consultations
Book Your Appointment
Get in Touch with Seawoods Hospital,
Navi Mumbai