Book Your Consultation With Nulife IVF Clinic
Share your details and our team will help you schedule an appointment with Navi Mumbai's best IVF Clinic
- Home
- / Our Specialities
- / Varicocelectomy
Varicocelectomy at Nullife IVF Clinic, Seawoods.
Advanced Surgical Solutions for Male Fertility in Navi Mumbai
What Is Varicocelectomy and Why Is It Done?
A varicocelectomy is a surgical procedure performed to correct a varicocele, which is an abnormal enlargement of the veins within the scrotum. Varicoceles can disrupt normal blood flow, raise scrotal temperature, and affect testicular function, sometimes leading to reduced sperm production, poor motility, or abnormal sperm shape.
The procedure involves tying off or sealing the affected veins, redirecting blood through healthy vessels. Varicocelectomy is done to:
- Improve sperm quality and male fertility
- Relieve discomfort or heaviness in the scrotum
- Prevent further testicular damage or shrinkage
- Support couples trying to conceive naturally or via assisted reproductive techniques
By addressing the root cause of vein enlargement, varicocelectomy not only eases symptoms but can also enhance reproductive potential, making it a key treatment for men facing fertility challenges related to varicoceles.
Why Choose Nullife IVF Clinic for Varicocelectomy Treatment in Navi Mumbai?
- Experienced Specialists: Our surgeons are skilled in microsurgical and laparoscopic varicocelectomy techniques, ensuring precise vein ligation and minimal tissue trauma. Microsurgical approaches in particular allow for faster recovery, reduced risk of recurrence, and lower complication rates.
- Integrated Fertility Team: Treatment is coordinated with our team of andrologists, urologists, and embryologists, ensuring that your varicocelectomy aligns with your overall fertility plan. We evaluate both partners as needed to provide a comprehensive approach to conception.
- Modern Facilities: Nullife IVF Clinic in Seawoods, Navi Mumbai, is equipped with advanced operating microscopes, sterile surgical suites, and high-quality diagnostic tools, ensuring optimal outcomes in a safe and hygienic environment.
- Personalized Support: From the initial consultation to post-operative follow-up, patients receive detailed guidance, emotional support, and counseling to understand the procedure, expected results, and next steps in fertility planning.
Varicocelectomy Work-Up in Seawoods, Navi Mumbai
A thorough evaluation is crucial before deciding on surgery. At our clinic, the process includes:
- Medical History & Physical Examination: Our specialists review symptoms, medical history, prior surgeries, lifestyle habits, and family history to assess potential contributing factors.
- Scrotal Ultrasound with Doppler: This imaging study evaluates the size of the veins, detects abnormal blood flow, and confirms the presence and grade of the varicocele.
- Semen Analysis: By measuring sperm count, motility, and morphology, we can determine whether the varicocele is affecting fertility. Multiple samples may be taken for consistency.
- Hormonal Testing: Testosterone, FSH, LH, and other hormones are checked to ensure the endocrine system is functioning normally. Any hormonal imbalances are addressed as part of the treatment plan.
- Fertility Counseling: Based on diagnostic results, our specialists explain the findings, discuss treatment options, and help patients make informed decisions about varicocelectomy or complementary fertility therapies.
Varicocelectomy Treatment Options at Nullife IVF Clinic
Depending on the severity, location, and patient preference, we offer several surgical options:
- Microsurgical Subinguinal Varicocelectomy: A small incision is made near the groin, and enlarged veins are tied under a microscope. This approach offers high precision, minimal post-operative pain, and rapid recovery.
- Laparoscopic Varicocelectomy: Performed through tiny incisions using a camera, this technique is ideal for large varicoceles or bilateral cases. Recovery is quick, and scarring is minimal.
- Open Inguinal Varicocelectomy: This traditional approach is chosen when patient anatomy or previous surgeries require direct access to the veins. Most procedures take approximately 30–60 minutes, and patients typically return home on the same day. Recovery is usually straightforward, with mild discomfort, bruising, or swelling that resolves within a few days to a week.
Post-Surgery Care and Recovery
Following varicocelectomy, patients are advised to:
- Avoid heavy lifting or strenuous activity for a few weeks.
- Wear supportive underwear to reduce discomfort.
- Follow prescribed medications and attend follow-up appointments.
- Monitor for complications such as infection, bleeding, or recurrence.
Most men notice a gradual improvement in scrotal discomfort within days and may see positive changes in sperm parameters within three to six months, supporting fertility potential.
Assisted Reproductive Techniques (ART) After Varicocelectomy
While surgery can improve sperm quality, some couples may still require ART to achieve pregnancy. Options include:
IUI (Intrauterine Insemination): Healthy sperm are prepared and placed directly into the uterus during ovulation to increase chances of fertilization.
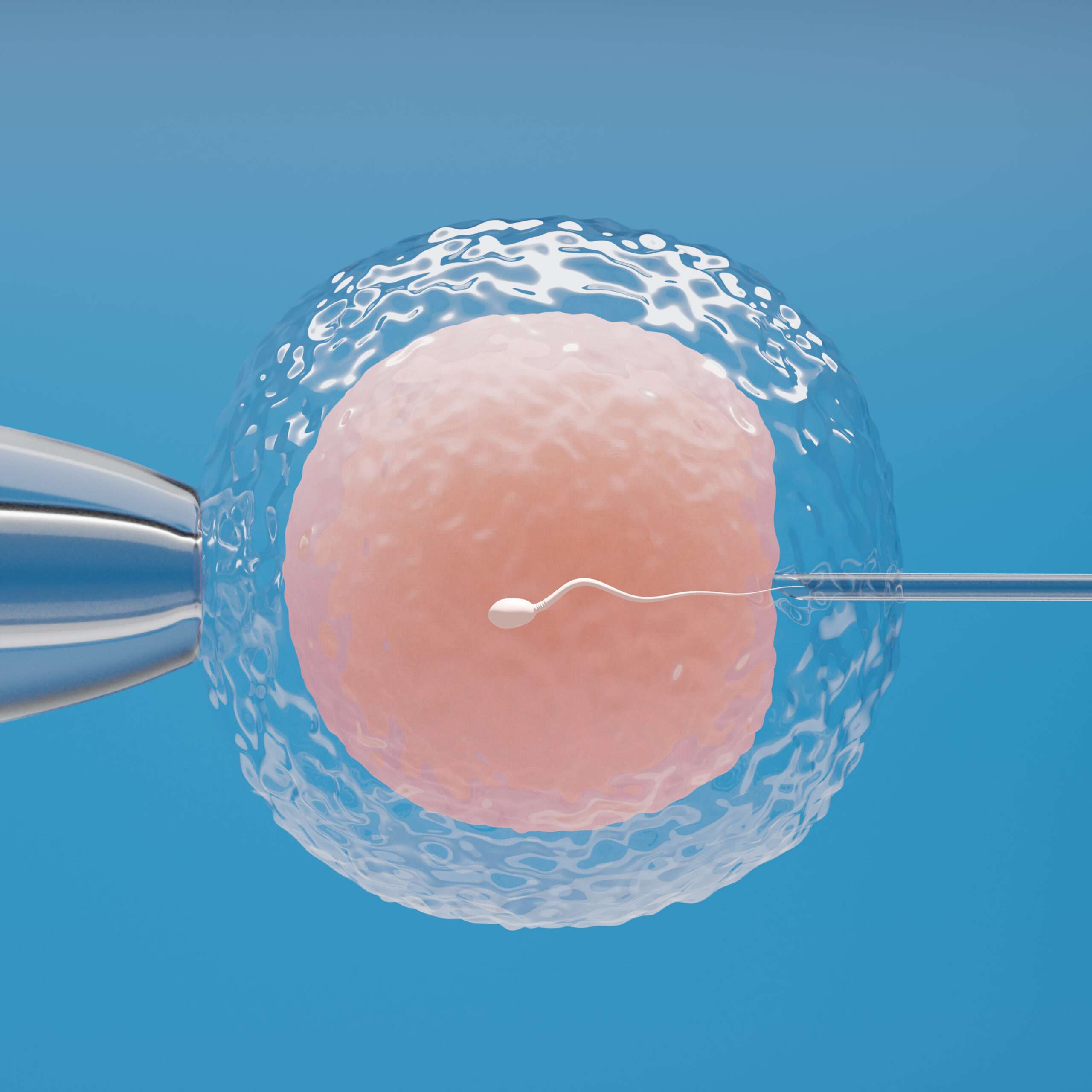
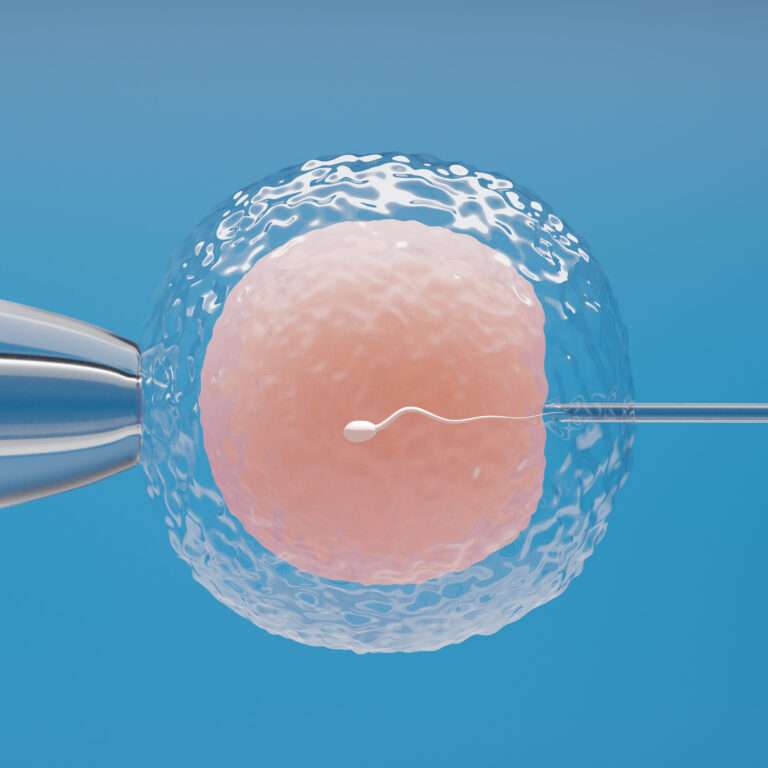
IVF (In Vitro Fertilization): Eggs are retrieved, fertilized in the laboratory, and healthy embryos are transferred into the uterus.
ICSI (Intracytoplasmic Sperm Injection): A single sperm is injected into an egg, which is particularly helpful in severe male infertility cases or after poor response to varicocelectomy.
Surgical Sperm Retrieval (TESA, TESE, PESA, MESA): If sperm is absent in semen despite surgery, advanced techniques allow direct collection from the testes or epididymis for use in IVF or ICSI.
Our fertility team integrates surgical outcomes with ART planning to provide a complete, personalized pathway toward parenthood.
Varicocelectomy at Nullife IVF Clinic offers a precise, effective solution for men experiencing varicoceles, discomfort, or fertility issues. Combined with a comprehensive evaluation, expert surgical techniques, and access to ART when necessary, our approach maximizes the potential for improved sperm quality and successful conception. With personalized support, modern facilities, and a skilled multidisciplinary team, patients receive high-quality care every step of the way.
Our Specialities
- Male infertility workup
- Female Infertility Work-up and Treatment
- IUI (intrauterine insemination)
- IVF (In Vitro Fertilization)
- ICSI (Intracytoplasmic Sperm Injection)
- Sperm Retrieval (TESA, TESE, PESA, MESA)
- Varicocelectomy
- Tuboplasty for Tubal Block
- Timed Intercourse
- Follicular / Ovulation Study
- Frozen Embryo Transfer (FET)
- Oocyte Retrieval
- View All Specialities
Hospital Locations
Nulife IVF, Seawoods, Navi Mumbai
Success Stories from Our Patients
Couples share their journey to parenthood with Nullife IVF Clinic.
I consulted Dr. Priyal for a IVF issue I had been anxious about for months, and I’m so glad I did. She made a sensitive topic easy to talk about...

Frequently Asked Questions About Sperm Retrieval
A varicocele is an abnormal enlargement of veins within the scrotum, similar to varicose veins in the legs. It can cause discomfort, a dragging sensation, or a “bag of worms” feeling above the testicle. Over time, it may affect testicular function, sperm production, motility, and overall fertility. Early detection and evaluation by a specialist can help prevent long-term damage.
Varicocelectomy is recommended when a varicocele causes pain, testicular shrinkage, or abnormal sperm parameters. The surgery corrects blood flow, reduces scrotal pressure, protects testicular health, and can significantly improve fertility outcomes, either for natural conception or assisted reproductive treatments.
The procedure is performed under local, spinal, or general anesthesia, so you won’t feel pain during surgery. Mild soreness, swelling, or bruising is common afterward but usually resolves within a few days. Pain medication is prescribed if needed.
Most men can resume light activities within 2–3 days. Strenuous exercise, heavy lifting, or sports are generally avoided for 2–4 weeks. Complete healing of tissues occurs gradually, and any discomfort diminishes as veins adapt to the new blood flow.
Varicocelectomy often leads to better sperm count, motility, and morphology over 3–6 months. While improvement varies per individual, studies show many men achieve higher chances of natural conception or improved outcomes with assisted reproductive techniques like IUI or IVF.
No overnight stay is usually necessary. Most varicocelectomy procedures are performed as day-care surgeries. You can typically go home a few hours after the procedure, provided vital signs are stable and post-operative instructions are clear.
Complications are uncommon but can include infection, bleeding, hydrocele (fluid collection around the testicle), or recurrence of the varicocele. Choosing an experienced microsurgeon and following post-operative care instructions significantly reduces these risks.
Recurrence is rare, especially with microsurgical subinguinal or laparoscopic techniques. Regular follow-up, including physical exams and semen analysis, helps detect and address any issues early if veins enlarge again.
Sexual activity can usually be resumed after 2–3 weeks, once swelling and discomfort subside. Your surgeon will confirm when it’s safe based on your healing and overall recovery.
Semen analysis is generally recommended at 3 and 6 months post-surgery to monitor improvements in sperm count, motility, and morphology. Results guide whether further fertility interventions are needed.
If azoospermia (no sperm in semen) is caused by a varicocele, surgery may restore sperm production. If not, advanced sperm retrieval techniques like TESA, TESE, or PESA may be considered for assisted reproductive treatments.
Yes. Our team provides comprehensive post-operative care including wound checks, repeat semen analysis, fertility counseling, and guidance on next steps toward conception. We ensure patients receive both medical and emotional support throughout their recovery.
Book Your Consultation for Fertility Treatment at Nullife IVF Clinic
A varicocele doesn’t have to limit your comfort or dreams of parenthood. With skilled surgeons, modern equipment, and an expert team, Nullife IVF Clinic in Seawoods, Navi Mumbai helps you get the best outcome from varicocelectomy and fertility treatment..
Your Guide to Male Fertility Care at Nullife IVF Clinic
Learn about advanced male fertility treatments, including IUI, IVF, and ICSI, designed to help couples achieve successful pregnancies at Nullife IVF Clinic.

ICSI (Intracytoplasmic Sperm Injection)
IVF (In Vitro Fertilization)

Fertility-Enhancing Endoscopic Surgeries
Get in Touch with Our Fertility Experts!
Contact Us for Appointments and Consultations
Book Your Appointment
Get in Touch with Seawoods Hospital,
Navi Mumbai